
Piriformis Syndrome
 Piriformis syndrome is a uncommon neuromuscular disorder. Piriformis syndrome is also known as "wallet sciatica" or "fat wallet syndrome," as the condition can be caused or aggravated by sitting with a large wallet in the affected side's rear pocket.
Piriformis syndrome is a uncommon neuromuscular disorder. Piriformis syndrome is also known as "wallet sciatica" or "fat wallet syndrome," as the condition can be caused or aggravated by sitting with a large wallet in the affected side's rear pocket.
Cause -
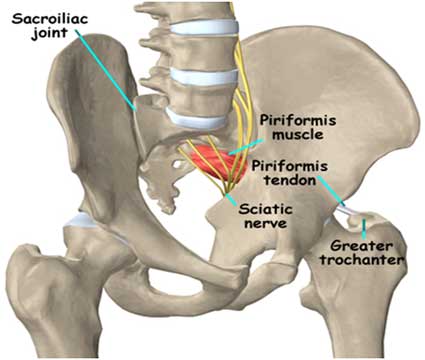
Piriformis - pear shaped, small, flat muscle in the buttock, it stabilizes the hip joint and lifts and rotates the thigh away from the body.
1. Piriformis syndrome typically occurs due to tightness of the piriformis muscle. This may occurs when the sciatic nerve is compressed or irritated by the piriformis muscle.
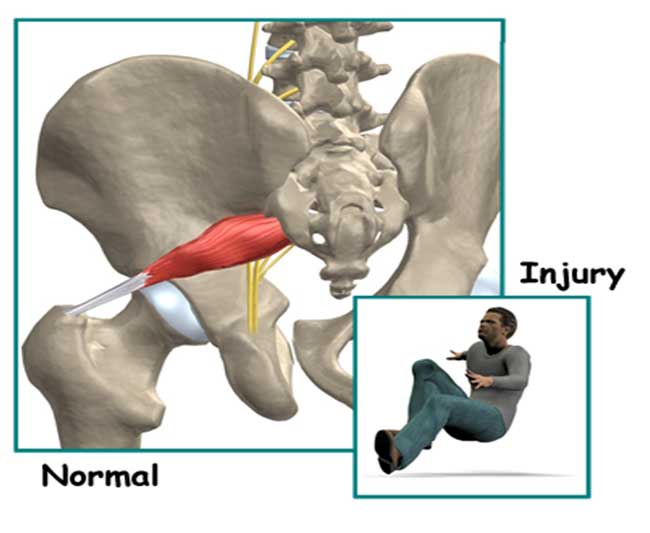
2. Piriformis Injury- the muscle may be injured due to a fall onto the buttock. Bleeding in and around the piriformis muscle forms a hematoma. A hematoma describes the blood that has pooled in that area. The piriformis muscle begins to swell and put pressure on the sciatic nerve. Soon the hematoma dissolves, but the muscle goes into spasm.
3. Overuse of the Piriformis
4. Injury to the lumbar spine
5. Due to repetitive strain or trauma
6. Sports or activities requiring repeated use of the Piriformis muscle. These activities may include:
• Running (especially changing direction)
• Sprinting
• Jumping
• Squatting
• Lunging
Symptoms -
1. Radiating pain in the buttock, posterior thigh and lower leg
2. The pain is exacerbated with activity, prolonged sitting, or walking.
3. Poor muscular biomechanics
4. Decreased ROM
5. Altered structural alignment
6. Decreased strength
7. Decrease endurance
8. Decrease motor coordination
9. Nerve Inflammation
10. Muscle Spasm
11. Tenderness in muscle
Diagnose -
1. CT scan
2. MRI
3. Ultrasound
4. EMG
5. Physical Examination -The Freiberg, the Pace, and the FAIR (flexion, adduction and internal rotation) maneuvers.
Contributing Factors -
1. Muscle tightness (particularly the piriformis and adductor muscles)
2. Joint stiffness (particularly the hip, lower back, sacroiliac joints or pelvic joints)
3. Muscle weakness (particularly the piriformis and gluteals)
4. Lower back injury
5. Poor posture
6. Excessive or inappropriate training
7. Poor biomechanics
8. Inadequate warm up
9. Poor pelvic or core stability
10. Muscle imbalances
Physiotherapy Treatment -
1. Soft tissue massage
2. Electrotherapy (e.g. ultrasound, swd, Ift)
3. Stretches
4. Muscle energy techniques
5. Joint mobilization
6. Neural mobilization
7. Ice or heat treatment
8. Postural education
9. Biomechanical correction
10. Progressive exercises to improve strength, flexibility and core stability
11. Activity modification advice
12. Devising and monitoring a return to sport or activity plan
13. Pulsed electromagnetic fields
14. Tolerance of positions and activities is increased Gait, locomotion, and balance are improved
15. Improve Motor function (motor control and motor learning)
16. Sensory awareness
17. Passive range of motion
18. Hot packs
19. McKenzie exercises
20. Myofacial release technique

