
Prolapsed Disc (Slipped Disc)
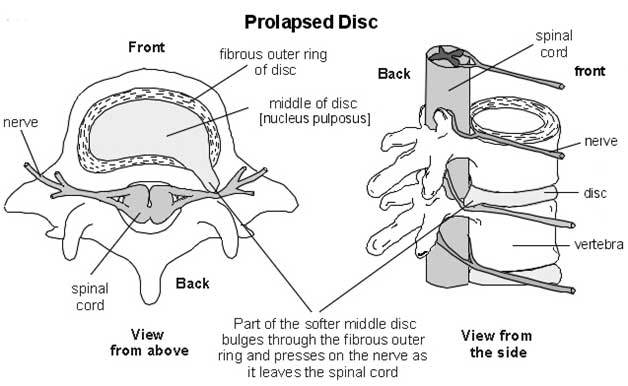
A prolapsed disc often causes severe lower back pain. The disc often presses on a nerve root which can cause pain. When you have a prolapsed disc (commonly called a slipped disc), a disc does not actually slip. What happens is that part of the inner softer part of the disc (the nucleus pulposus) bulges out (herniates) through a weakness in the outer part of the disc. A prolapsed disc is sometimes called a herniated disc. The bulging disc may press on nearby structures such as a nerve coming from the spinal cord. Some inflammation also develops around the prolapsed part of the disc.
Cause -
 Various things may trigger the inner softer part of the disc to prolapse out through the weakened outer part of the disc.
Various things may trigger the inner softer part of the disc to prolapse out through the weakened outer part of the disc.
For example-
1. Sneezing
2. Awkward bending
3. Heavy lifting in an awkward position may cause some extra pressure on the disc
In people with a weakness in a disc, this may be sufficient to cause a prolapse. Factors that may increase the risk of developing a prolapsed disc include:
1. A job involving lots of lifting
2. A job involving lots of sitting (especially driving)
3. Weight-bearing sports (weight lifting, etc)
4. Smoking
5. Obesity
6. Increasing age (a disc is more likely to develop a weakness with increasing age)
Large number of people has shown that some people have a prolapsed disc without any
Symptoms. It is thought that symptoms mainly occur if the prolapse causes pressure on
irritation of nerve.
Sign and Symptom -
1. Low back pain
2. Numbness
3. Tingling
4. Muscular weakness
5. Paralysis
6. Paresthesia
7. Affection of reflexes
8. Muscle spasm
9. Cauda equine syndrome - Compression of the cauda equina can cause permanent nerve damage or paralysis. The nerve damage can result in loss of bowel and bladder control as well as sexual dysfunction. This disorder is called cauda equina syndrome.
Location -
Cervical
Lumbar
Investigation -
1. X-ray
2. Computed tomography scan (CT or CAT scan)
3. Magnetic resonance imaging (MRI)
4. Myelogram
5. Electromyogram and Nerve conduction studies (EMG/NCS)
6. Transcranial Magnetic Stimulation (TMS)
Treatment -
Patient education on proper body mechanics
Non-steroidal anti-inflammatory drugs (NSAIDs)
Oral steroids (e.g. prednisone or methylprednisolone)
Epidural cortisone injection
Intravenous sedation, analgesia-assisted traction therapy (IVSAAT)
Weight control
Tobacco cessation
Physiotherapy -
1. Physical therapy, to address mechanical factors, and may include modalities to temporarily relieve pain (i.e. traction, electrical stimulation)
2. Lumbosacral back support
3. Spinal manipulation: spinal manipulation is more effective than placebo for the treatment of acute (less than 3 months duration) lumbar disk herniation and acute sciatica. spinal manipulation is safe when used by appropriately-trained practitioners," and spinal manipulation is safe for the treatment of disk-related pain. But it is contraindicated in cauda equine syndrome.
4. Electro stimulation
5. Laser Light Therapy
6. Ultrasound Therapy
7. Hot/Cold Therapy
8. Weightlifting

